Emerging research is illuminating a surprising connection between chronic gastrointestinal disorders—particularly irritable bowel syndrome (IBS)—and the long-term risk of neurodegenerative diseases like Alzheimer’s and Parkinson’s. Once thought to be isolated to the digestive tract, conditions like IBS are now being re-evaluated as potential early warning signs of brain health decline.
At the heart of this discovery lies the gut-brain axis—a complex network linking the central nervous system with the enteric nervous system of the gut. This bidirectional communication system involves neural, hormonal, and immune pathways, allowing the gut to influence brain function and vice versa.
Recent studies suggest that chronic inflammation, microbial imbalances (dysbiosis), and intestinal permeability—common features in IBS—may trigger systemic inflammation that reaches the brain. Over time, this low-grade inflammation could contribute to the development of neurodegenerative conditions.
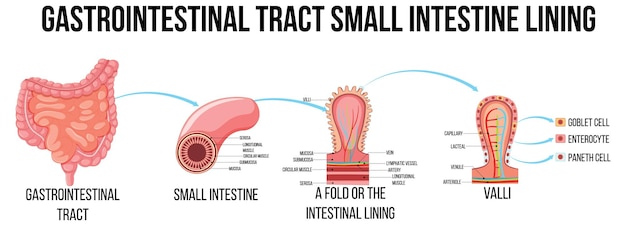
The gut-brain axis connects digestive health with cognitive and neurological function.
A new body of evidence suggests that individuals with IBS may face a higher risk of developing Alzheimer’s and Parkinson’s diseases later in life. While correlation does not imply causation, the consistency of findings across multiple studies has prompted scientists to explore IBS not just as a digestive issue, but as a systemic condition with neurological implications.
One study highlighted that people with IBS and vitamin D deficiency—a common comorbidity—showed biomarkers associated with early neurodegeneration. Vitamin D plays a role in immune regulation and neuroprotection, and its deficiency may amplify inflammation in both the gut and brain.
Beyond IBS, research has identified four specific gastrointestinal disorders associated with an increased risk of Parkinson’s disease: inflammatory bowel disease (IBD), constipation, gastroparesis, and small intestinal bacterial overgrowth (SIBO). Notably, gastrointestinal symptoms often appear years—or even decades—before motor symptoms of Parkinson’s emerge.
Scientists now hypothesize that abnormal proteins, such as alpha-synuclein, may originate in the gut and travel to the brain via the vagus nerve, a key component of the gut-brain axis. This so-called 'body-first' theory of Parkinson’s is gaining traction and could reshape how we approach early detection.

Emerging theory suggests Parkinson’s may start in the gut before affecting the brain.
Genetic studies have also linked chronic pain and poor mental well-being to an increased risk of IBS, suggesting overlapping biological pathways. These findings point to the importance of integrated care that addresses both gastrointestinal and psychiatric health.
Stress, anxiety, and depression are known to exacerbate IBS symptoms, but they may also independently contribute to neuroinflammation and neurodegeneration. This overlap underscores the need for holistic treatment approaches that consider the whole person, not just isolated symptoms.
The rise in IBS and chronic idiopathic constipation during the COVID-19 pandemic further highlights the interplay between stress, infection, and gut health. SARS-CoV-2 can directly infect gut cells, potentially disrupting the microbiome and triggering long-term gastrointestinal issues. Combined with pandemic-related stress, these factors may have accelerated gut dysfunction in vulnerable individuals.
While no direct link has been established between post-COVID gut symptoms and neurodegeneration, the prolonged inflammation and dysbiosis observed raise concerns about long-term neurological consequences.
These findings open new avenues for early intervention. Monitoring individuals with chronic gut disorders for cognitive and motor changes could allow for earlier diagnosis of Alzheimer’s or Parkinson’s. Additionally, managing gut health through diet, probiotics, and anti-inflammatory treatments may offer protective benefits for the brain.
Interestingly, lifestyle factors such as coffee consumption, tea intake, and physical activity—once thought to influence IBS—showed no consistent causal relationship in recent genetic studies. This suggests that while lifestyle plays a role, the underlying biology of IBS and its neurological links may be more complex than previously thought.
As research continues to unravel the connections between gut health and brain disease, one message is clear: the digestive system may be a critical window into neurological well-being. Recognizing IBS and related conditions not just as discomforts, but as potential red flags, could transform how we approach brain health in the future.
By integrating gastroenterology, neurology, and mental health care, we may be able to detect and mitigate neurodegenerative risks long before symptoms appear—offering hope for more effective prevention strategies.

Health

Health

Health

Health

Health

Health

Health

Health

Health

Health

Health

Health

Health

Fitness

Health

Health