Alzheimer’s disease affects millions worldwide, with late-onset forms being the most common. While age and lifestyle play roles, genetics increasingly emerge as critical players. One gene, PICALM, has long been associated with increased risk for late-onset Alzheimer’s disease (LOAD). Recent research now reveals a surprising and specific role for a PICALM risk allele in microglia—the brain’s primary immune cells—particularly in how they manage fat storage. This discovery opens new doors to understanding how lipid metabolism in brain immunity contributes to neurodegeneration.
PICALM, short for Phosphatidylinositol Binding Clathrin Assembly Protein, is involved in clathrin-mediated endocytosis—a cellular process crucial for transporting molecules across cell membranes. In neurons, PICALM helps regulate synaptic vesicle recycling and the internalization of amyloid precursor protein (APP), potentially influencing the production of amyloid-beta, a hallmark protein in Alzheimer’s pathology.
Genome-wide association studies (GWAS) have consistently flagged PICALM as one of the top genetic risk factors for LOAD, second only to APOE. However, the exact mechanisms by which PICALM variants increase risk remained unclear—until recently.
Microglia, the brain's immune sentinels, are now at the center of Alzheimer's genetic research.
New studies have revealed that a specific PICALM risk allele—commonly inherited and associated with higher Alzheimer’s risk—does not act uniformly across brain cells. Instead, its impact is most pronounced in microglia.
Microglia are responsible for maintaining brain health by clearing cellular debris, pathogens, and abnormal proteins like amyloid-beta. When these cells become dysfunctional, it can accelerate neurodegeneration. The PICALM risk variant appears to disrupt normal lipid metabolism within microglia, leading to the accumulation of lipid droplets—fatty storage organelles typically associated with metabolic stress.
Lipid droplets are not inherently harmful—they play roles in energy storage and membrane synthesis. But in chronic inflammatory or stressed environments, such as those seen in aging brains or neurodegenerative conditions, excessive lipid droplet accumulation can impair cell function.
In microglia carrying the PICALM risk allele, researchers observed a significant increase in lipid droplets, especially in response to amyloid-beta exposure. This suggests that the gene variant compromises the cell’s ability to process and clear fats efficiently, leading to a buildup that may trigger inflammatory responses and reduce the microglia’s capacity to protect neurons.
This lipid accumulation is not just a side effect—it appears to be a functional consequence of disrupted endocytic trafficking. Since PICALM is involved in membrane dynamics, its dysfunction may impair the transport of lipid-processing enzymes or receptors, trapping fats inside the cell.
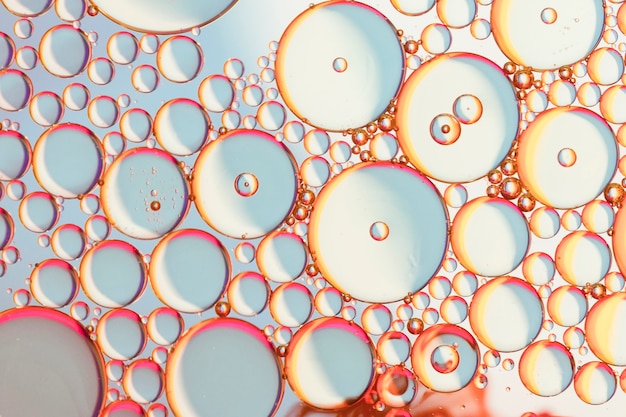
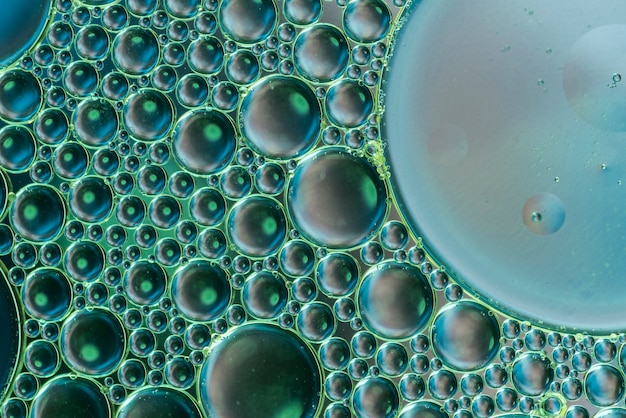
Microscopic view showing lipid droplets (stained) accumulating in microglia with the PICALM risk variant.
The link between PICALM, lipid droplets, and Alzheimer’s progression involves a cascade of events:
This pathway highlights how a single genetic variant can have cell-type-specific effects with far-reaching consequences. It also shifts focus from neurons alone to the broader brain ecosystem, where immune and metabolic health are equally vital.
Understanding the role of PICALM in lipid regulation opens new avenues for treatment. Rather than targeting amyloid plaques alone, future therapies might aim to restore lipid homeostasis in microglia. Potential strategies include:
Moreover, this discovery emphasizes the importance of personalized medicine. Genetic screening for PICALM and related variants could help identify individuals at higher risk long before symptoms appear, enabling early intervention.
The finding that a PICALM allele drives lipid droplet accumulation in microglia represents a paradigm shift in Alzheimer’s research. It underscores the complexity of the disease, where genetics, immunity, and metabolism intersect in unexpected ways.
As scientists continue to unravel the roles of risk genes in specific cell types, we move closer to precise, effective treatments. For now, this research reminds us that protecting the brain may require more than just clearing plaques—it may mean keeping our brain’s immune cells metabolically fit.

Health

Health

Health

Health

Health

Health

Health

Health

Health

Health

Health

Health

Fitness

Health

Health