Gut Health as a Window to Brain Disease: IBS and Other Chronic Conditions May Signal Alzheimer’s and Parkinson’s Risk
Emerging research is revealing a powerful connection between chronic health conditions—particularly gastrointestinal disorders like irritable bowel syndrome (IBS)—and the long-term risk of neurodegenerative diseases such as Alzheimer’s and Parkinson’s. What happens in the gut may, in fact, be an early warning sign for what could unfold in the brain years later.
A growing body of evidence suggests that disruptions in the gut-brain axis—the bidirectional communication network linking the digestive system and the central nervous system—could play a pivotal role in the development of neurodegenerative conditions. This insight is reshaping how scientists and clinicians view early detection and prevention strategies for diseases once thought to originate solely in the brain.
The Gut-Brain Connection: More Than Just a Theory
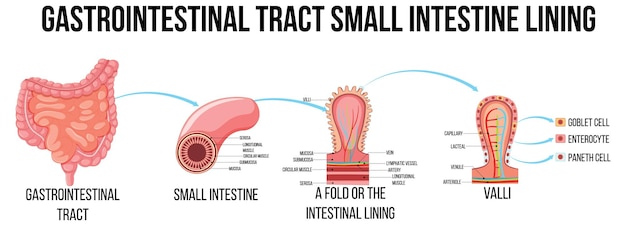
The human gut is home to trillions of microbes that influence digestion, immunity, and even mood. But recent studies show this complex ecosystem may also impact brain health. The vagus nerve, inflammatory markers, and microbial metabolites are all pathways through which gut disturbances could signal or even contribute to neurological decline.
One compelling study highlighted that individuals with IBS, chronic constipation, and other gastrointestinal disorders exhibit a higher incidence of Parkinson’s disease later in life. In fact, gastrointestinal symptoms such as constipation often appear years—sometimes decades—before motor symptoms of Parkinson’s become evident.
IBS and Neurodegeneration: What the Data Shows
While IBS has long been associated with abdominal pain, bloating, and irregular bowel habits, its implications may extend far beyond the digestive tract. Researchers analyzing large health datasets have found that people diagnosed with IBS are more likely to develop both Alzheimer’s and Parkinson’s diseases over time.
This correlation appears to be more than coincidental. Shared mechanisms such as chronic inflammation, dysbiosis (an imbalance in gut bacteria), and impaired intestinal barrier function (often referred to as 'leaky gut') are common features in both IBS and neurodegenerative disorders. These conditions may create a systemic environment conducive to neuronal damage.
Other Chronic Conditions That May Predict Brain Health
IBS is not alone in its potential to signal future brain disease. The same studies point to several other chronic conditions that may serve as early indicators:
- Chronic pain: Persistent pain conditions, including fibromyalgia and migraines, are linked to both IBS and increased neurodegenerative risk, possibly due to shared neural sensitization pathways.
- Mental well-being: Depression, anxiety, and chronic stress are strongly associated with IBS and have also been identified as risk factors for Alzheimer’s and Parkinson’s.
- Vitamin D deficiency: Low levels of vitamin D, common in people with gastrointestinal disorders, are independently linked to cognitive decline and Parkinson’s progression.
- Autoimmune and inflammatory bowel diseases: Conditions like Crohn’s disease and ulcerative colitis also show elevated associations with Parkinson’s, reinforcing the inflammation-neurodegeneration link.

The Role of Lifestyle and Environment
Interestingly, recent genetic studies have explored modifiable risk factors for IBS, including diet and behavior. While factors like coffee consumption, tea intake, and physical activity did not show consistent causal links to IBS, chronic pain and mental health emerged as key targets for prevention.
The pandemic further underscored this connection: during the peak of COVID-19, there was a significant rise in IBS and chronic idiopathic constipation, likely driven by both viral impacts on the gut and heightened psychological stress. This surge highlights how environmental stressors can trigger or worsen gut conditions—potentially setting the stage for long-term neurological consequences.
Implications for Early Detection and Prevention
If gastrointestinal and other chronic conditions can serve as early biomarkers for neurodegenerative disease, this opens new avenues for intervention. Monitoring patients with IBS, especially those with additional risk factors like chronic pain or mood disorders, could allow for earlier neurological screening and lifestyle modifications.
Potential preventive strategies include anti-inflammatory diets, probiotics to support gut microbiome balance, stress reduction techniques like mindfulness, and regular monitoring of vitamin D levels. While these approaches are not cures, they may help mitigate risk or delay onset.
Looking Ahead
The idea that gut health may predict brain health is no longer speculative—it’s becoming a cornerstone of integrative medicine. As research continues to unravel the complex interplay between the body’s systems, the importance of a holistic approach to health becomes ever clearer.
Future studies may focus on identifying specific microbial signatures or inflammatory markers in IBS patients that correlate most strongly with neurodegeneration. This could lead to blood or stool tests capable of estimating an individual’s risk years in advance.
For now, the message is clear: taking care of your gut may be one of the most important things you can do for your brain.









