When Ozempic hit the market seven years ago, it was primarily hailed as a breakthrough for managing type 2 diabetes. Over time, its remarkable ability to promote weight loss catapulted it into the public spotlight, reshaping conversations around obesity treatment. But the story of GLP-1 receptor agonists doesn’t end there. These drugs are now emerging as powerful tools in the fight against a range of chronic conditions—from heart and liver disease to potentially even neurodegenerative disorders like Alzheimer’s.
GLP-1 (glucagon-like peptide-1) receptor agonists are a class of medications originally developed to help regulate blood sugar in people with type 2 diabetes. They work by mimicking the action of the natural GLP-1 hormone, which stimulates insulin release, suppresses glucagon, slows gastric emptying, and increases satiety. Drugs like Ozempic (semaglutide), Trulicity, and Victoza have proven effective not only in glucose control but also in promoting significant weight reduction.
The weight loss benefits of these medications led to the development of Wegovy, a higher-dose version of semaglutide specifically approved for chronic weight management. This success has opened the door to exploring broader therapeutic applications.
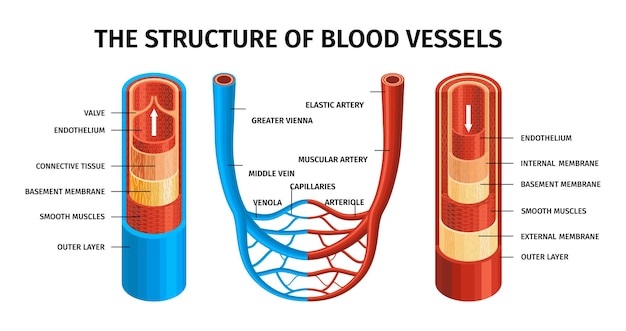
One of the first major expansions beyond diabetes was in cardiovascular disease. Clinical trials revealed that GLP-1 drugs significantly reduce the risk of major adverse cardiovascular events—such as heart attack, stroke, and cardiovascular death—in patients with type 2 diabetes who are at high risk.
This cardioprotective effect is believed to stem from a combination of improved metabolic control, reduced inflammation, blood pressure lowering, and direct effects on heart tissue. As a result, GLP-1 receptor agonists are now recommended in treatment guidelines for patients with type 2 diabetes and established heart disease.
Non-alcoholic fatty liver disease (NAFLD) and its more severe form, non-alcoholic steatohepatitis (NASH), affect millions worldwide and are closely linked to obesity and insulin resistance. Until recently, treatment options were limited to lifestyle changes.
Emerging research shows that GLP-1 drugs can reduce liver fat, inflammation, and fibrosis in patients with NASH. Semaglutide, in particular, has demonstrated promising results in clinical trials, improving liver histology and potentially slowing disease progression. While not yet approved specifically for liver disease, these findings suggest a transformative role for GLP-1 agonists in hepatology.

Now, the most ambitious frontier for GLP-1 drugs is neuroscience. Novo Nordisk, the manufacturer of Ozempic and Wegovy, has launched clinical trials to investigate whether semaglutide can slow the progression of Alzheimer’s disease.
This isn’t a far-fetched hypothesis. Alzheimer’s has long been referred to as 'type 3 diabetes' due to insulin resistance in the brain, which may contribute to cognitive decline and neurodegeneration. GLP-1 receptors are present in the brain, particularly in areas involved in memory and learning. Preclinical studies in animal models have shown that GLP-1 agonists can reduce neuroinflammation, decrease amyloid plaque buildup, and improve synaptic function.
Human observational studies have also been encouraging. People with type 2 diabetes who take GLP-1 drugs appear to have a lower risk of developing dementia compared to those on other diabetes medications. While these findings are associative and not conclusive, they provide a strong rationale for controlled trials.
The potential mechanisms are multifaceted:
If clinical trials confirm these benefits, GLP-1 drugs could become the first disease-modifying treatments for Alzheimer’s—offering hope to millions affected by this devastating condition.
Despite the excitement, challenges remain. GLP-1 drugs can cause gastrointestinal side effects such as nausea, vomiting, and diarrhea, which may be poorly tolerated in older adults. Long-term safety data in non-diabetic populations, especially for cognitive applications, is still limited.
Additionally, access and cost are significant barriers. These medications are expensive, and widespread use for chronic conditions like Alzheimer’s would require substantial healthcare investment and policy reform.
The expanding applications of GLP-1 drugs represent a paradigm shift in medicine—one where a single therapeutic pathway can address multiple interconnected diseases rooted in metabolism and inflammation.
As research continues, scientists are also exploring next-generation GLP-1 agonists, dual and triple receptor agonists (such as those targeting GIP and glucagon), and improved delivery methods to enhance efficacy and tolerability.
The journey from diabetes management to potential Alzheimer’s treatment underscores the importance of continued investment in metabolic research. What began as a tool for blood sugar control may ultimately redefine how we treat some of the most challenging diseases of the 21st century.
The story of GLP-1 drugs is still being written—and the next chapter could be the most groundbreaking yet.

Health

Health

Health

Health

Health

Health
Health

Health

Health

Health

Health

Health

Health

Fitness

Health

Health