A deep dive into the science of pain and the powerful non-pharmacological tools reshaping how we manage it.

Pain is universal. Whether it's a stubbed toe, chronic backache, or post-surgical discomfort, everyone experiences it. But what if our understanding of pain — and how we treat it — is undergoing a revolutionary shift? A groundbreaking new book is challenging conventional wisdom by exploring not just why we feel pain, but how the mind can play a pivotal role in managing it.
At the heart of this exploration is a compelling argument: pain is not just a physical signal from damaged tissue. It's a complex experience shaped by emotions, attention, memory, and context. This new perspective opens the door to innovative, non-drug strategies — including distraction and meditation — as powerful tools in the pain management toolkit.
For decades, pain was seen as a straightforward alarm system: tissue damage occurs, nerves send signals to the brain, and the brain registers pain. But modern neuroscience reveals a far more intricate process.
Pain is not a direct measure of injury. Instead, it's the brain's interpretation of potential threat. Two people with identical injuries can experience vastly different levels of pain — influenced by stress, expectations, past experiences, and even cultural background. This explains why soldiers have reported walking on broken limbs during battle, or why anxiety can amplify a minor ache.
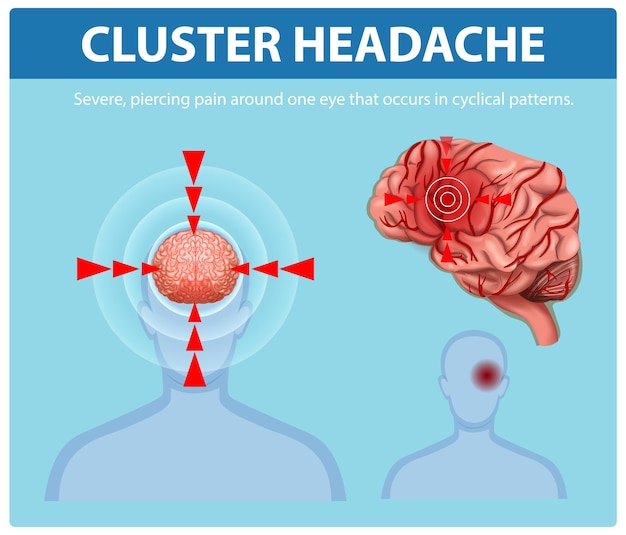
Understanding pain as a perception — not just a sensation — changes everything. The brain doesn’t just receive pain; it constructs it. This means that altering brain activity can directly influence how pain is felt.
Technologies like functional MRI have shown that practices such as meditation and focused attention can reduce activity in pain-processing regions of the brain. These techniques don’t erase the source of pain, but they change how the brain responds to it — effectively turning down the volume.
Distraction is one of the oldest and most accessible pain management techniques. Whether it’s a child focusing on a toy during a shot or an athlete pushing through fatigue, shifting attention away from pain can reduce its intensity.
Studies have shown that engaging in cognitively demanding tasks — such as solving puzzles, playing video games, or listening to immersive music — can significantly reduce reported pain levels. This isn’t just psychological trickery; brain scans confirm decreased activation in pain-related areas when attention is redirected.
The mechanism is simple: the brain has limited attentional resources. When focus is directed elsewhere, fewer mental 'bandwidth' is available to process pain signals. This makes distraction especially effective for acute pain and procedural discomfort.
While distraction diverts attention, meditation transforms the relationship with pain. Mindfulness meditation, in particular, teaches individuals to observe pain without judgment or resistance. Instead of fighting the sensation, practitioners learn to acknowledge it with curiosity and acceptance.
Research has demonstrated that regular meditation can lead to structural changes in the brain — increasing gray matter in areas linked to emotional regulation and decreasing activity in regions associated with threat detection. Over time, this can reduce both the intensity and emotional distress of chronic pain.
Unlike medication, meditation doesn’t mask pain. It empowers individuals to respond differently — reducing fear, anxiety, and the tendency to catastrophize, all of which can worsen pain perception.

The growing recognition of these techniques has led to their integration into clinical settings. Cognitive-behavioral therapy (CBT), mindfulness-based stress reduction (MBSR), and biofeedback are now common components of pain management programs.
These approaches are particularly valuable in addressing chronic pain conditions — such as fibromyalgia, lower back pain, and neuropathy — where traditional treatments often fall short. They offer sustainable, side-effect-free methods to improve quality of life.
None of this suggests that medication or surgery should be abandoned. For many conditions, they remain essential. But the new understanding of pain emphasizes the need for a multidisciplinary approach — one that combines physical treatment with psychological and neurological strategies.
Patients are increasingly encouraged to take an active role in managing their pain. Learning techniques like meditation or using distraction during painful procedures empowers individuals and reduces dependency on pharmaceuticals.
As research continues to uncover the complexities of pain, the line between physical and mental health grows thinner. The future of pain care lies in personalized, integrative models that treat the whole person — not just the symptom.
Books exploring these ideas are helping to shift public perception and encourage open conversations about non-traditional therapies. With greater awareness, techniques like meditation and distraction may become as routine in pain clinics as ice packs and painkillers.
Pain doesn’t have to be endured in silence or managed solely with pills. By understanding the brain’s role in shaping our experience, we gain new tools — and new hope — for relief.

Health

Health

Health

Health

Wellness

Wellness
Health

Health

Wellness

Wellness

Wellness

Wellness

Health

Fitness

Health

Health