A groundbreaking new study has uncovered a precise biological mechanism linking a well-known autism-associated gene mutation to disruptions in social behavior. Researchers have discovered that mutations in the SHANK3 gene—a genetic alteration linked to autism spectrum disorder (ASD) and Phelan-McDermid syndrome—interfere with the brain’s ability to release vasopressin, a critical neuropeptide involved in social bonding and communication.
This discovery marks a pivotal step in understanding the neurobiological roots of social challenges in autism and opens new doors for targeted therapies.
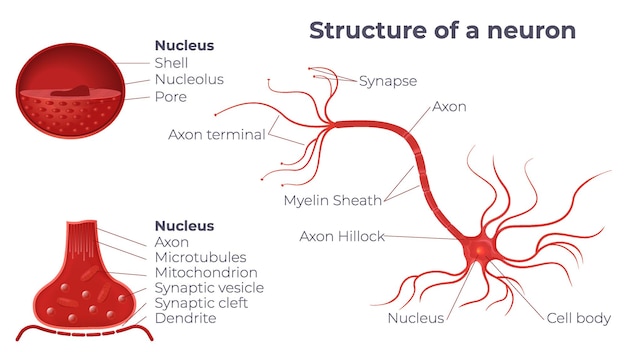
The SHANK3 gene provides instructions for making a protein that acts as a scaffold in the synapses—the junctions where neurons communicate. This protein helps organize other molecules that transmit signals between nerve cells, particularly in regions of the brain involved in cognition, emotion, and social behavior.
Mutations in SHANK3 have long been associated with neurodevelopmental disorders. Individuals with deletions or damaging mutations in this gene often exhibit core symptoms of autism, including impaired social interaction, delayed speech, and repetitive behaviors. However, until now, the exact pathway from gene mutation to altered behavior remained unclear.
Vasopressin is a neuropeptide produced in the hypothalamus and released into various brain regions. While it's widely known for regulating water balance and blood pressure, recent research has highlighted its crucial role in social behaviors such as pair bonding, trust, aggression, and social recognition—functions often altered in autism.
Animal studies have shown that manipulating vasopressin levels can significantly influence social interaction. For example, increasing vasopressin in the brain enhances social memory and affiliation in rodents. Conversely, blocking its receptors leads to social withdrawal.
The new study, conducted using genetically modified mouse models, revealed that SHANK3 mutations specifically impair the function of neurons that produce vasopressin. These neurons, located in the hypothalamus, showed abnormal electrical activity and reduced ability to release vasopressin in response to social stimuli.
Further investigation showed that the SHANK3 protein is essential for maintaining the structural integrity of synapses on vasopressin-producing neurons. Without functional SHANK3, these synapses become unstable, disrupting the signaling cascade that triggers vasopressin release.
Mice with SHANK3 mutations exhibited significant deficits in social behavior. They spent less time interacting with unfamiliar mice, showed reduced interest in social odors, and failed to recognize previously encountered peers—behaviors analogous to social impairments seen in humans with autism.
Critically, when researchers administered vasopressin directly into the brain, these social deficits were reversed. The treated mice showed normalized social interaction, suggesting that the behavioral changes were directly linked to vasopressin deficiency rather than broader developmental issues.
This study is the first to directly link a genetic cause of autism to a specific neurochemical pathway involving vasopressin. It suggests that therapies aimed at boosting vasopressin signaling could be beneficial for individuals with SHANK3-related autism.
Clinical trials are already exploring the use of intranasal vasopressin in children with autism. Early results show modest improvements in social communication, but this new research provides a biological rationale for why such treatments might work—and for which subgroups they may be most effective.
Moreover, the findings highlight the importance of personalized medicine in autism. Since autism is a spectrum with diverse genetic causes, treatments may need to be tailored to specific biological subtypes. Individuals with SHANK3 mutations could represent a subgroup most likely to respond to vasopressin-based therapies.
Researchers now aim to explore whether other autism-linked genes also affect vasopressin or related neuropeptide systems. Understanding common downstream pathways could lead to broader therapeutic strategies that benefit multiple genetic subtypes.
Additionally, non-invasive methods to measure vasopressin levels in the human brain are being developed, which could help identify patients who would benefit most from targeted treatments.
The discovery that SHANK3 mutations disrupt vasopressin release offers a clear mechanistic link between a genetic defect and social behavior in autism. By pinpointing this pathway, scientists are moving closer to biologically informed treatments that address the root causes of social challenges, rather than just managing symptoms.
As research continues to unravel the complex biology of autism, studies like this underscore the power of neuroscience to transform our understanding—and treatment—of neurodevelopmental conditions.

Health

Health

Health

Health

Health
Health

Health

Health
Health

Health

Health

Fitness

Health

Health