Herpes simplex virus (HSV) affects over 400 million people globally, causing lifelong infections with no known cure. Despite decades of research, effective prevention and treatment options remain limited. However, a groundbreaking discovery involving a neutralizing nanobody that targets the prefusion conformation of HSV glycoprotein B (gB) is offering new hope. This tiny but powerful molecule not only blocks viral entry but also shows cross-species activity, opening doors to broad-spectrum antiviral strategies.
Herpes simplex virus exists in two main forms: HSV-1, commonly associated with oral herpes, and HSV-2, which primarily causes genital herpes. Both types establish latent infections in nerve cells, periodically reactivating to cause symptoms. The virus enters host cells through a complex fusion process mediated by viral envelope glycoproteins.
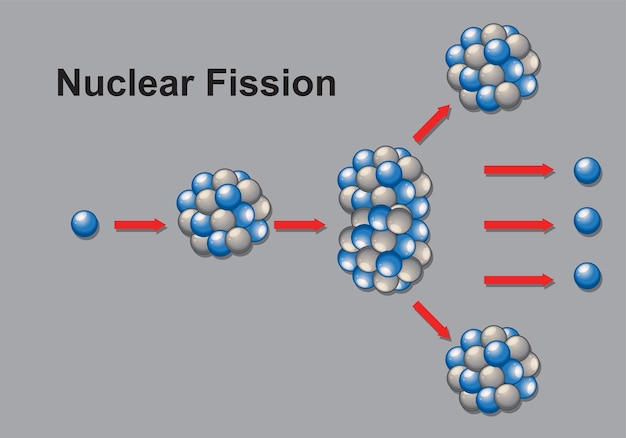
Among these glycoproteins, glycoprotein B (gB) plays a central role as the fusogen—the protein responsible for merging the viral envelope with the host cell membrane. For fusion to occur, gB must undergo a structural shift from a prefusion to a postfusion state. Targeting gB in its prefusion conformation—before it triggers membrane fusion—has emerged as a promising strategy to stop the virus in its tracks.
Nanobodies are antibody fragments derived from the immune systems of camelids, such as llamas and alpacas. Unlike conventional antibodies, nanobodies are much smaller, more stable, and capable of binding to hidden or transient protein structures—like the prefusion form of gB—that traditional antibodies often miss.
Researchers have now isolated a nanobody that specifically recognizes and locks gB in its prefusion state. By doing so, it prevents the structural rearrangement necessary for membrane fusion, effectively neutralizing the virus before it can enter human cells.
One of the most exciting aspects of this nanobody is its cross-species activity. It has demonstrated the ability to neutralize HSV not only in human cell cultures but also in animal models across different species. This suggests a high degree of conservation in the prefusion gB structure among herpesviruses, raising the possibility that this nanobody—or similar ones—could be effective against other members of the herpesvirus family, such as Epstein-Barr virus or cytomegalovirus.
Such broad reactivity enhances its potential as a universal antiviral agent and strengthens its value in both therapeutic and preventive applications.
The discovery of this nanobody also provides critical insights into vaccine development. By stabilizing the prefusion conformation of gB, scientists can now use this structure as a blueprint for designing next-generation immunogens—molecules that elicit a protective immune response.
Vaccines based on the prefusion gB could train the immune system to produce antibodies that mimic the nanobody’s action, blocking viral entry before infection takes hold. This approach mirrors recent successes in vaccine design for respiratory syncytial virus (RSV) and SARS-CoV-2, where prefusion-stabilized proteins led to highly effective vaccines.
Beyond vaccines, this nanobody represents a direct antiviral intervention. Due to its small size and stability, it could be developed into a topical microbicide—such as a gel or cream—to prevent HSV transmission during sexual contact. Alternatively, it could be engineered for systemic delivery to treat active outbreaks or suppress reactivation in immunocompromised individuals.
Its specificity for the prefusion gB minimizes off-target effects, making it a safer candidate compared to broad-acting antivirals like acyclovir, which can lead to resistance over time.
While promising, several challenges remain. Long-term safety, delivery methods, and large-scale production must be addressed before clinical use. Additionally, researchers must determine whether the virus can mutate to escape nanobody neutralization—a common hurdle in antiviral therapy.
Ongoing studies are exploring engineered versions of the nanobody with enhanced potency and half-life. Combination therapies—pairing the nanobody with other antivirals or immune modulators—may further improve efficacy and reduce resistance risks.
The identification of a nanobody that neutralizes HSV by targeting the prefusion form of glycoprotein B marks a major advance in virology. Its cross-species activity, mechanistic clarity, and therapeutic versatility make it one of the most promising tools in the fight against herpesviruses.
As research progresses, this discovery could pave the way for new vaccines, preventive strategies, and treatments that finally offer long-term control—or even elimination—of herpes infections worldwide.

Health

Health

Health

Health

Health

Fitness

Health

Health